Dexpanthenol is an alcohol derivative of pantothenic acid, a component of the B complex vitamins and an essential component of a normally functioning epithelium.
Dexpanthenol is an alcohol derivative of pantothenic acid, a component of the B complex vitamins and an essential component of a normally functioning epithelium. Discovered by Roger J. Williams in 1933, it is a water-soluble vitamin. More than 70 years ago, the first topical dexpanthenol-containing formulation has been developed. Nowadays, various topical dexpanthenol preparations exist, tailored according to individual requirements. Topical dexpanthenol has emerged as frequently used formulation in the field of dermatology and ophthalmology.
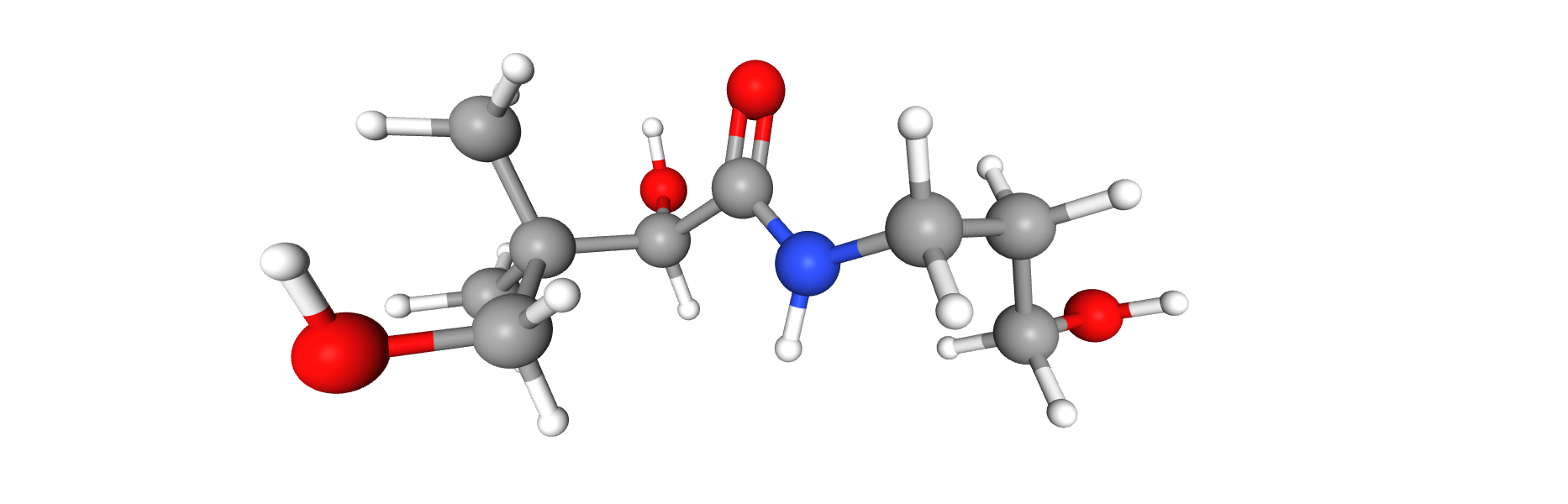
Dexpanthenol is enzymatically cleaved to form pantothenic acid, which is an essential component of Coenzyme A, which acts as a cofactor in many enzymatic reactions that are important for protein metabolism in the epithelium. Coenzyme A serves as a cofactor for a variety of enzyme-catalyzed reactions involving the transfer of acetyl groups. By increasing the synthesis of coenzyme A, mitochondrial coenzyme A is also increased which leads to more ATP synthesis. ATP and coenzyme A are indispensable for synthesis of phospholipids and cholesterol, which again have a role in repair of cell membranes.
Regarding the Dexpanthenol, while pantothenic acid is optically active, only the dextrorotatory form (dexpanthenol) is biologically active. The name “pantothenic acid” is derived from the Greek word “pantothen”, which means “from everywhere” and a small amount of it is present in almost every food (legumes, whole grain cereals, eggs, meat, avocado and curd).
Dermatological effects of the topical use of dexpanthenol include increased fibroblast proliferation and accelerated re-epithelialization in wound healing. It normalizes cellular metabolism, increases the strength of collagen fibres, has a weak anti-inflammatory effect.
Different topical dexpanthenol preparations exist (cream, emollient, drops, gel, lotion, oil, ointment, solution and spray), tailored according to individual needs, ranging from pediatric to adult use. For these reasons, it has a widely known toxicity profile. The mechanisms by which dexpanthenol restores and protects skin barrier function have not been fully elucidated. However, in 2009, an in vitro study demonstrated the molecular mechanisms of pantothenate on the proliferation of dermal fibroblasts.
Is compared to untreated cells, treated fibroblasts showed a significant upregulation of some cytokines. As IL-6 and IL-8 are among the cytokines most strongly expressed during wound healing,
the upregulation of IL-6 and IL-8 expression in dermal fibroblasts further supports the fact that dexpanthenol containing topical ointments contribute to the wound healing. At the same time, as the different layers of the skin undergo continual renewal, moisturizers provide an environment, which promotes physiological processes necessary for maintaining or restoring skin barrier function.
In the ophthalmology field, Dexpanthenol plays an important role in healing of the conjunctival and corneal epithelial damage. Due to its hygroscopic nature, it prevents epithelial dryness and maintains the ocular surface integrity.
Dexpanthenol acts like a moisturizer and hydrating agent, keeping the ocular surface comfortable. It improves the hydration when applied topically, this activity may be related to dexpanthenol’s hygroscopic properties and its capability to promote retention of moisture. The hydrating effect seems to be interrelated with its capacity to regenerate the epidermal barrier.
Several studies demonstrated that, in the treatment of corneal micro-injuries of cornea, Dexpanthenol ophthalmic formulation significantly reduces the duration of treatment due to the shortening of the membrane restoration period. Moreover, it was demonstrated that, if the efficacy of tear substitutive therapy is insufficient, the use of dexpanthenol is recommended since it is an effective preparation for surface defects of the epithelial layer and contributes to rapid epithelialization due to its ability to stimulate the process of migration of epithelial cells to the damage zone, as well as to stimulate their proliferation.
Bibliography:
• Changes in the tear film and ocular surface from dry eye syndrome, Johnson ME and Murphy PJ, Progr in Retinal and Eye Res, 2004:23, 449-474.
• Post-LASIK dry eye. Roni M Shtein. Expert Rev Ophthalmol. 2011 October ; 6(5): 575–582
• Tear film and ocular surface tests in animal models of dry eye: uses and limitations, Barabino S, Chen W and Dana MR., Exp Eye Res, 2004: 79, 613-621.
• Artificial tear solutions, Lemp MA, Int Ophthalmol Clin 1973:13, 221-9
• Menoapuse and dry eye. A possible relationship, Versura P, Campos EC, Gynecol ENdocrinol. 2005 May; 20(5): 289-98, Review.
• TFOS DEWS II Report Executive Summary. Jennifer P. Craig, J. Daniel Nelson, Dimitri T. Azar, Carlos Belmonte, Anthony J. Bron, Sunil K. Chauhan, Cintia S. de Paiva, Jos e A.P. Gomes, Katherine M. Hammitt, Lyndon Jones, Jason J. Nichols, Kelly K. Nichols, Gary D. Novack, Fiona J. Stapleton, Mark D.P. Willcox, James S. Wolffsohn, David A. Sullivan. The Ocular Surface (2017)


