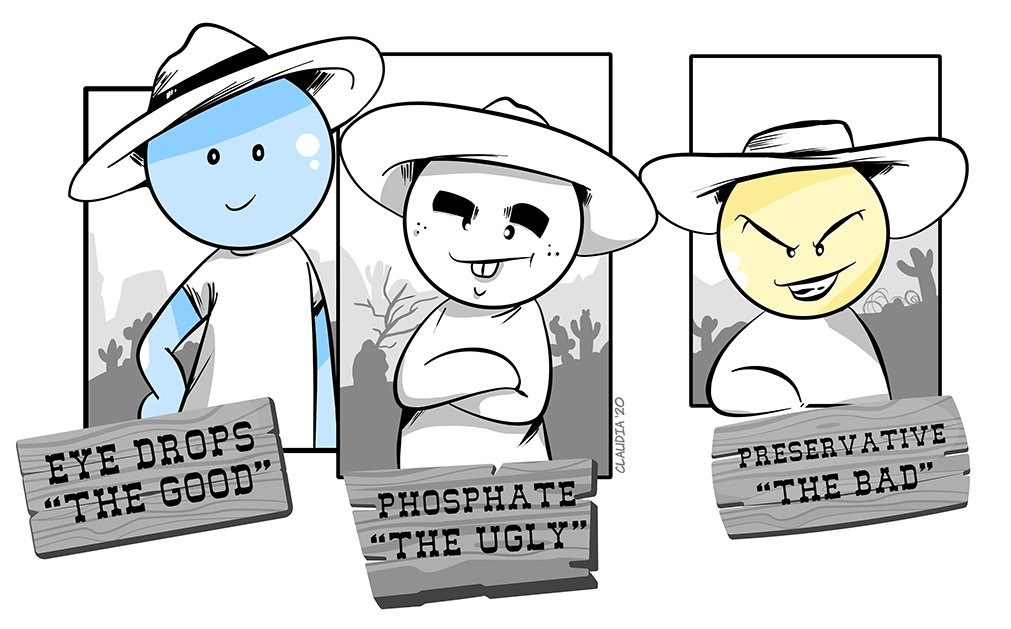
OPHTHALMIC FORMULATIONS: THE GOOD, THE BAD AND THE UGLY
Phosphate, preservatives and other excipients constitute the majority of the total volume of a medicine. They ensure the safety and efficacy of the drugs, but their toxicity is not a simple issue for several reasons.
Excipients constitute about 90% of the total volume of a medicine. The most important action of any excipient is to ensure the safety and efficacy of the drugs throughout the formulation, the storage period, and during and after its administration.
The toxicity of excipients (intrinsic or specific toxicity) is not a simple issue for several reasons: first, the large number of excipients and their diversity of chemical profiles or sources or technological functions and second the presence or probability of occurrence of secondary products and contaminants.
Nowadays, pharmaceutical excipients are more than just simple elements added to complete a total volume formulation; these substances require numerous guarantees to the safety and efficacy of the drug, such as ensure stability throughout the formulation process to the administration of the medicine by the patient. They also may guarantee that the dose is administered and delivered with the same precision and accuracy established for that API in particular, thus making the medicine administration more adequate and reflecting positive results in terms of patient adherence to therapy.
The Bad: Preservative
The need for sterility in multidose eyedrops requires the inclusion of an antimicrobial preservative in the solutions, most frequently the quaternary ammonium benzalkonium chloride (BAK), and offer the advantages of decreasing the likelihood of contamination in multidose containers and prolonging shelf life.

Some patients on long-term treatments experience allergic or inflammatory reactions. Those may include redness, stinging, burning, irritation, eye dryness, or less frequently conjunctivitis or corneal damage. For example, many studies indicate a direct correlation between the presence of preservatives and the symptoms experienced during antiglaucoma therapy.
The same issue for dry eye management the potential for bacterial contamination in artificial tear agents is a real-world issue and the topic of frequent debate.
Two main preservative categories exist for this function in eye solutions: detergent preservatives and the more recently developed oxidative preservatives. Detergent preservatives alter cell membrane permeability by causing lipid dispersion and lysis of cytoplasmic contents. In contrast, oxidative preservatives work by penetrating cell membranes and interfering with intracellular reactions.
The nonspecificity of preservatives presents a difficult challenge; we need them to eradicate potentially harmful bacteria, yet associated with their utility exists the potential for ocular cytotoxicity.
Long-term use of detergent-preserved artificial tears increases the likelihood of adverse effects, including damage to the epithelial surface and decreased tolerability due to irritation, which may adversely affect compliance. In particular, studies have shown that increased exposure to benzalkonium chloride is an independent risk factor for the development of ocular surface disease. Moreover, the development of cataract have been associated with the use of preservative medications, probably due to Benzalkonium Chloride.
Benzalkonium Chloride is a potent preservative linked with possible side effects:
Many clinical trials showed that Benzalkonium Chloride alone, and to a much lesser extent latanoprost or timolol, strongly stimulated the expression by lens epithelial cells of soluble mediators involved in inflammatory and, or apoptotic processes, (prostaglandin E2, interleukin-1a, and interleukin-6). These mediators could, therefore, favour or stimulate lens opacification.
Benzalkonium chloride is recognised to destabilise the tear film lipid layer through its detergent-like tensioactive effects, which may promote excessive evaporation of the aqueous tear film. Furthermore, the pro-inflammatory and toxic effects of preservatives can also lead to chronic damage to the ocular surface and disrupt tear film homeostasis.

Benzalkonium chloride (BAK)
The toxic effects of BAK are time and dose-dependent, such that in small enough quantities, the harmful effects are often well tolerated. It is when patients require multiple medications taken multiples times per day that the adverse effects add up and lead to more severe reactions on the ocular surface.
For example, various human studies demonstrated reduced goblet cell density and increased conjunctival inflammation, with the use of preserved eye solutions dosed two or four times per day for three months.Also, patients with compromised tear film may be at higher risk for BAK-induced tear film instability.
The oxidative transient preservatives:
As an alternative to detergent preservatives, oxidative transient preservatives were developed. These preservatives dissipate upon contact with the eye, reducing the risk of ocular surface damage.
The stabilized oxychloro complex (SOC) present in Purite dissipates by converting into components usually found in tear. However, transient preservatives may still possess mild ocular toxicity.
Preferred Practice Pattern Dry Eye Syndrome Medical Treatment guidelines (prepared by the American Academy of Ophthalmology Cornea/External Disease Panel) recommend that patients with suggestive symptoms of dry eye be placed on trial treatments of artificial tears, with preservative-free artificial tear substitutes if used more than 4-6 times per day.
Preservative-free tear substitutes are as efficient as preserved tears, and they avoid the adverse ocular effects that may be induced by the non-specificity of preservatives. Non-preserved artificial tears are safe to use as often as needed and do not contribute to preservative overload, which allows practitioners and patients increased flexibility of use. This is especially critical when considering the heterogeneity of dry eye syndrome sufferers.
The Ugly: Phosphate Buffer
Buffers exist in all ophthalmic preparations to maintain a constant pH to prevent decomposition of active drugs and control tonicity. The most common buffer systems used in ophthalmic formulations are citrate, phosphate, Tris-HCl (Tris), and borate buffer. As phosphate naturally occurs in the eye, it has been the buffer of choice for a long time.
Since the buffer capacity is regulated by its concentration, some formulations use higher dosages to enhance the drug’s performance. The concentration of phosphate in tested artificial tears ranges from
A study demonstrated that 44% of the products revealed phosphate concentrations above the physiological level (1.45 mM), and in 5% of the products, there were phosphate concentrations higher than 50 mM.
Within the antiglaucoma medications, 47% of the formulations showed phosphate concentrations higher than the physiological level, and 19% had concentrations above 100 mM. The concentrations of the tested devices ranged from

Scientific studies demonstrated that chronic use of the phosphate buffer could cause corneal calcification:
Various scientific studies demonstrated that the phosphate buffer, used chronically, could cause corneal calcification. Calcification occurs when calcium cations and phosphate anions form insoluble crystal within the tissue. In the cornea, deposit typically occurs as hydroxyapatite. Phosphate buffers in drops occur at higher strengths than the physiological concentration in the tear fluid.
Has been estimated that it would require 20.4 days to form total corneal calcifications between the calcium in tears and unlimited phosphate. Deposition of calcium can be observed as a spectrum of clinical findings, ranging from subtle age-related superficial changes to full-thickness calcification of the entire cornea with visual loss. Both superficial band keratopathy and deeper calcareous calcification have been linked to the presence of phosphate excipients in topical ophthalmic medicines.
There are several case studies in which calcific band keratopathy, a calcific degeneration of the superficial cornea characterized by calcium hydroxyapatite deposition, has appeared after instilling phosphate buffer contained in ophthalmic medicinal products. Especially in eye drops applied after corneal injuries, studies show that the buffer composition influences the healing process and the development of corneal calcification.
The European Medicines Agency (EMA) has concluded that patients with ocular surface disease are at highest risk. Instead, the literature report no complications after the application of citrate, borate, and Tris buffering systems in humans.
Taking a combination of two or more drugs, for those who are at risk of undergoing surgery, and for all patients who will need treatments over several decades, preservative-free and phosphate-free formulations would provide clinically relevant benefits and should become a gold standard in ocular pharmacology.
Bibliography:
• Catia G. Abrantes, Dinah Duarte, Catarina P. Reis. An Overview of Pharmaceutical Excipients: Safe or Not Safe? Journal of Pharmaceutical Sciences 105 (2016) 2019e2026
• Penny A. Asbell (2006) Increasing importance of dry eye syndrome and the ideal artificial tear: consensus views from a roundtable discussion, Current Medical Research and Opinion, 22:11, 2149-2157,
• G.C. M. Rossi; C. Tinelli, G. Pasinetti; G. Milano and P. E. Bianchi; Dry eye syndrome-related quality of the life in glaucoma patients. European Journal of Ophthalmology Vol.19 n.4, 2009, pg. 572-579
• M. Banitt, H. Jung; Ocular Surface Disease in the glaucoma patient. International Ophthalmology Clinics, Vol. 58, N. 3, 2018, pg.23-33
• Christophe Baudouin, Antoine Labbé, Hong Liang, Aude Pauly, Françoise Brignole-Baudouin. Preservatives in eyedrops: The good, the bad and the ugly. Progress in Retinal and Eye Research 29(2010), pgg. 312e334
• W. Bernauer, M.A. Thiel, U.M. Langenauer, K.M. Rentsch; Phosphate concentration in artificial tears, Graefe’s Arch Clin Exp Ophthalmol (2006) 244: 1010-1014;
• Nadine Schuerer, Elisabeth Stein, Aleksandra Inic-Kanada, Marion Pucher, Christine Hohenadl, Nora Bintner, Ehsan Ghasemian, Jacqueline Montanaro and Talin Barisani-Asenbauer; Implications for ophthalmic formulations: ocular buffers show varied cytotoxic impact on human corneal–limbal and human conjunctival epithelial cells; Cornea, Volume 36, Number 6, June 2017
• Bernauer W, Thiel MA, Rentsch KM. Phosphate concentrations in antiglaucoma medication. Klin Monbl Augenheilkd. 2007;224:249–251.
• W. Bernauer, M.A. Thiel, M. Kurrer, A. Heiligenhaus, K.M. Rentsch, A. Schmitt, C. Heinz, A. Yanar; Corneal calcification following intensified treatment with sodium hyaluronate artificial tears; Br J. Ophthalmol 2006; 90: 285-288;
• Popiela MZ, Hawkswort N. Corneal calcification and phosphates: do you need to prescribe phosphate free?; Journal of ocular pharmacology and therapeutics, vol. 30, n° 10, 2014:800-802;


