THE IMPORTANCE OF VITREOUS BODY
The vitreous body is a relevant component of the eyeball. Keep it good health is important because any change in its structure or composition may affect the vision or lead to more severe pathology.
The vitreous body is the clear gel that fills the space between the crystalline lens and the retina, and represents about the 2/3 of the ocular volume. It is composed of a transparent, non-vascularized, gelatinous connective tissue that is surrounded by a membrane called the cortex.
The vitreous gel is 98% water, while for 1% collagen fibres, sugars, vitreous cells, called hyalocytes; proteins, hyaluronic acid, electrolytes, etc. these elements constitute the scaffolding, organized in an exquisitely clear gel. The collagen fibres are suspended in a network of glucosaminoglycans, long linear double sugars chains, and thickened by hyaluronic acid.

The vitreous humour has multiple functions:
• Mechanical: it contributes to the support of the eye;
• Trophic: promotes nutrition of the retinal tissue;
• Optics: allows valid transmission of light to the retina.
Structural changes in the vitreous can affect the vision and lead to more severe pathology:

Structural changes within the vitreous body can have many causes such as: inflammation, vitreoretinal dystrophies, myopic and diabetic vitreopathy, but most commonly result from ageing.
In addition to altering the internal structure of the vitreous body, ageing also weakens vitreoretinal adhesion. Age-related degenerations of the vitreous body begin at 20 to 30 years old but occur after 40-50. However, in myopic subjects, the clinical signs are anticipated by at least ten years before.
Gel liquefaction results from molecular alterations with the dissociation of collagen from hyaluronan and aggregation of collagen fibrils forming fibres, that cause light scattering and hence symptomatic floaters, especially in myopia.
With ageing, gel liquefaction and weakened vitreoretinal adhesion result in Posterior Vitreous Detachment (PVD), the most common cause of primary symptomatic floaters arising from the dense collagen matrix of the posterior vitreous cortex.

Recent studies indicate that symptomatic floaters are not only more prevalent but also have a negative impact on the quality of life that is greater than previously appreciated.
Primary vitreous floaters that result from myopia or age-related degeneration, and secondary floaters, usually from vitreous haemorrhage or uveitis, are at times highly symptomatic and can significantly impact on vision and quality of life.
Vitreous degeneration begins with the fluidization of its gelatinous component that leads to the formation of synchysis, i.e. lacunae of vitreous liquefaction composed of hyaluronic acid and water.
The synchysis destabilizes the vitreous body and promotes the syneresis, that is its collapse. If the corneal liquefaction progresses, there is a loss of the mechanical supporting function of the vitreous body. A subsequent reduction of the vitreous volume by contraction of the collagen fibres leads to the progressive detachment of the vitreous from the retina.
The synchysis destabilizes the vitreous body and promotes the syneresis, that is its collapse. If the corneal liquefaction progresses, there is a loss of the mechanical supporting function of the vitreous body. A subsequent reduction of the vitreous volume by contraction of the collagen fibres leads to the progressive detachment of the vitreous from the retina.
The cause that initiates the liquefaction of the vitreous gel is not known.
It is believed that metabolic changes and photochemical damage are involved with the production of free oxygen radicals that cause conformational changes of vitreous macromolecules. And, those changes lead to the dissociation of collagen from hyaluronic acid and the consequent formation of Vitreous liquid that results in a posterior vitreous detachment (PVD).
PVD abnormalities can manifest themselves in various ways. In the periphery of the ocular fundus, advanced liquefaction of the gel in the presence of strong vitreoretinal adhesion causes retinal breaks and detachments.
At the optic disc level, abnormal PVD can induce various vitreous-papillopathies as well as having an active role in neovascularization and vitreous haemorrhage in ischemic retinopathies. On the macula, abnormal PVD can cause a variety of pathologies, depending on whether the vitreous cortex is intact (thickness) or divided (partial thickness-vitreoschysis).
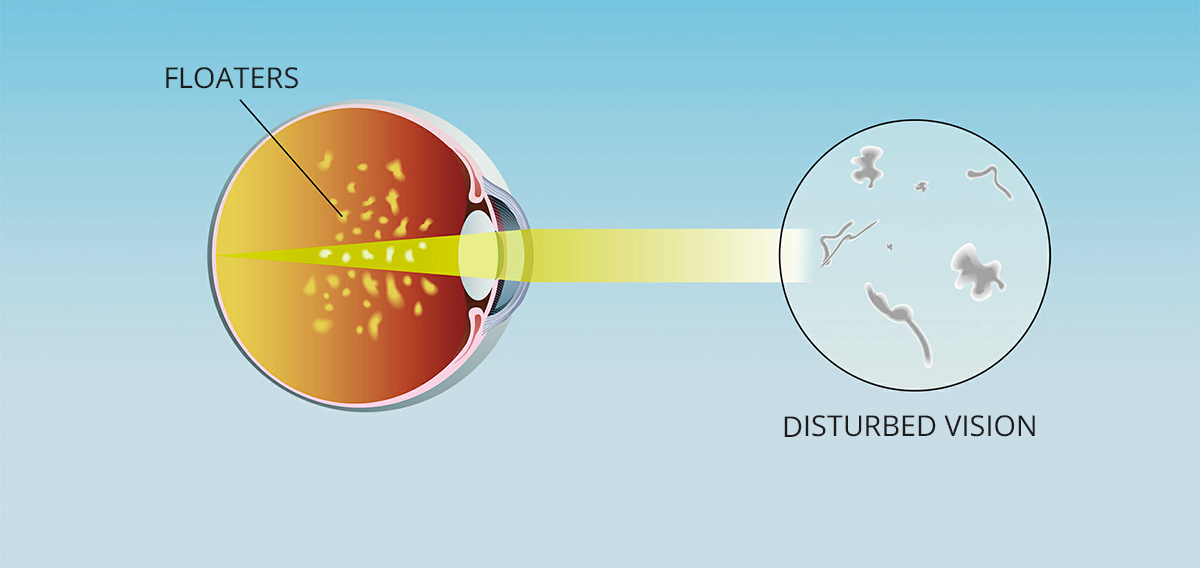
After 40 years old there is a steady increase in observed liquid vitreous associated with a decrease in gel volume so that by the age of 80±90 years, more than half of the vitreous is liquified. And myopia is associated with more rapidly progressive vitreous liquefaction. A progressive imbalance of the aqueous or molecular component of the vitreous leads to deterioration of the gelatinous structure with the formation of particular mobile filaments (floaters and flashing lights).
Treatment and prevention
Currently, there are no specific drugs for the treatment of vitreous floaters. Surgical removal of the vitreous, called "vitrectomy", can eliminate the floaters but, this procedure is undoubtedly disproportionate to the risks that it entails, and also is unjustified remove all the structural functions that the vitreous performs to treat this disease.
In clinical practice is widely acknowledged a support prevention therapeutic intervention, based on amino acids, vitamins and mineral salts. As such, preventive treatment may counteract the biochemical mechanisms underlying the degeneration of the vitreous and maintain the physiological composition of the vitreous gel.
Indeed the amino acids, more specifically carnitine, lysine and arginine allow the formation of type II collagen, a substance highly present at the level of the vitreous. Moreover, the B group vitamins (B1, B2, B6 and B12) are significant cofactors in all specific metabolic reactions at intravitreal level.
It is also advisable to follow a diet rich in fruits and vegetables and low in animal fat, and drink plenty of water to counteract the depletion of the water component of the vitreous.
Bibliography:
• Structural Macromolecules and Supramolecular Organization of the Vitreous Gel, P.N. Bishop; Progress in Retinal and Eye Research Vol. 19, No. 3, pp. 323 to 344, 2000;
• Matrix metalloproteinase biology applied to vitreoretinal disorders, C.S. Sethi, T.A.Bailey, P.J.Luthert, N. H.V. Chong; Br J Ophthalmol 2000; 84: 654-666;
• Safety of Vitrectomy for Floaters, H. S.Tan, M.Mura, S.Y. Lesnik Oberstein, H.M. Bijl; American Journal of Ophthalmology, June 2011, Vol.151 n.6; 995-998;
• Distribution of free amino acids in human intraocular fluids. Davis G. Durham. Tr. Am. Ophth. Soc. Vol. 68, 1970;
• Enzymatic Degradation Identifies Components Responsible for the Structural Properties of the Vitreous Body. Benjamen A. Filas, Qianru Zhang, Ruth J. Okamoto, Ying-Bo Shui and David C.
• Vitreous Floaters: Etiology, Diagnostics, and Management. Rebecca Milston, Michele C. Madigan, J. Sebag; Survey of Ophthalmology (2016), doi: 10.1016/j.survophthal.2015.11.008


